Make easier with a patient advocate.
Solace advocates fight for the treatments, approvals, and care you deserve.
Covered by Medicare nationwide.
Covered by Medicare in all 50 states














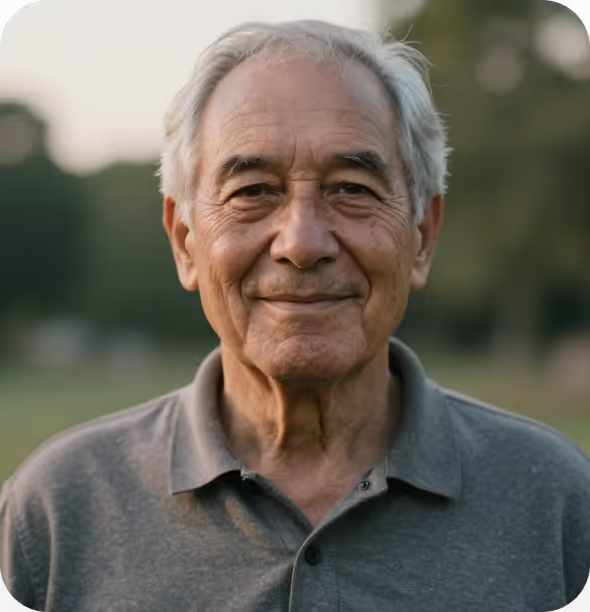
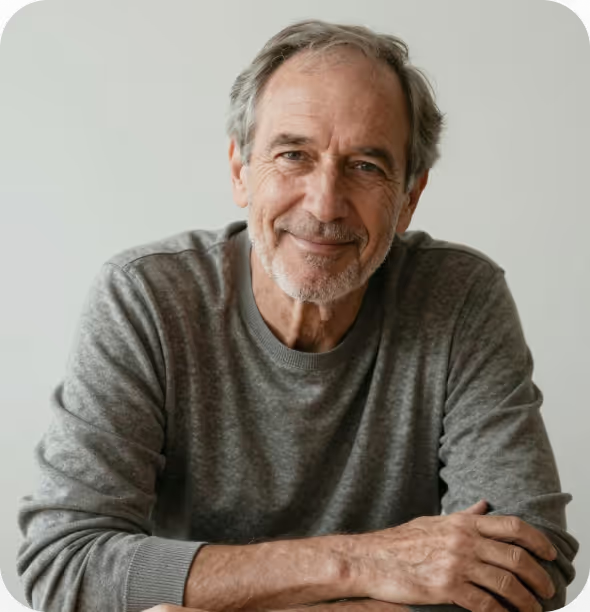
Advocates Fight for the Care You Deserve
You stay focused on your health. We’ll handle the healthcare system.

How it Works
- 1
Tell us what's important
From the start, you’ll be heard. Our physician will listen to your challenges and help you choose your advocate.
- 2
Meet your advocate
This is your turning point. You’ll meet your dedicated advocate and make a plan to get the care you need.
- 3
Support that stays with you
Your advocate helps as long as you need—staying in touch, guiding your care, and dramatically improving your quality of life.
Your Care, Your Way
Connect by video, phone, text, or email—whatever works best for you.




Caring for a loved one?
A Solace advocate works alongside your family to manage your loved one’s care.
Get expert healthcare support with...
- Doctors
- Decisions
- Planning



Alexa and Hilary
Daughters of a Solace Patient


Don’t navigate healthcare alone.
200,000 patients and families already trust Solace to deliver better care. You deserve an advocate.